SMC1A related Developmental and Epileptic Encephalopathy (SMC1A DEE)
SMC1A Gene
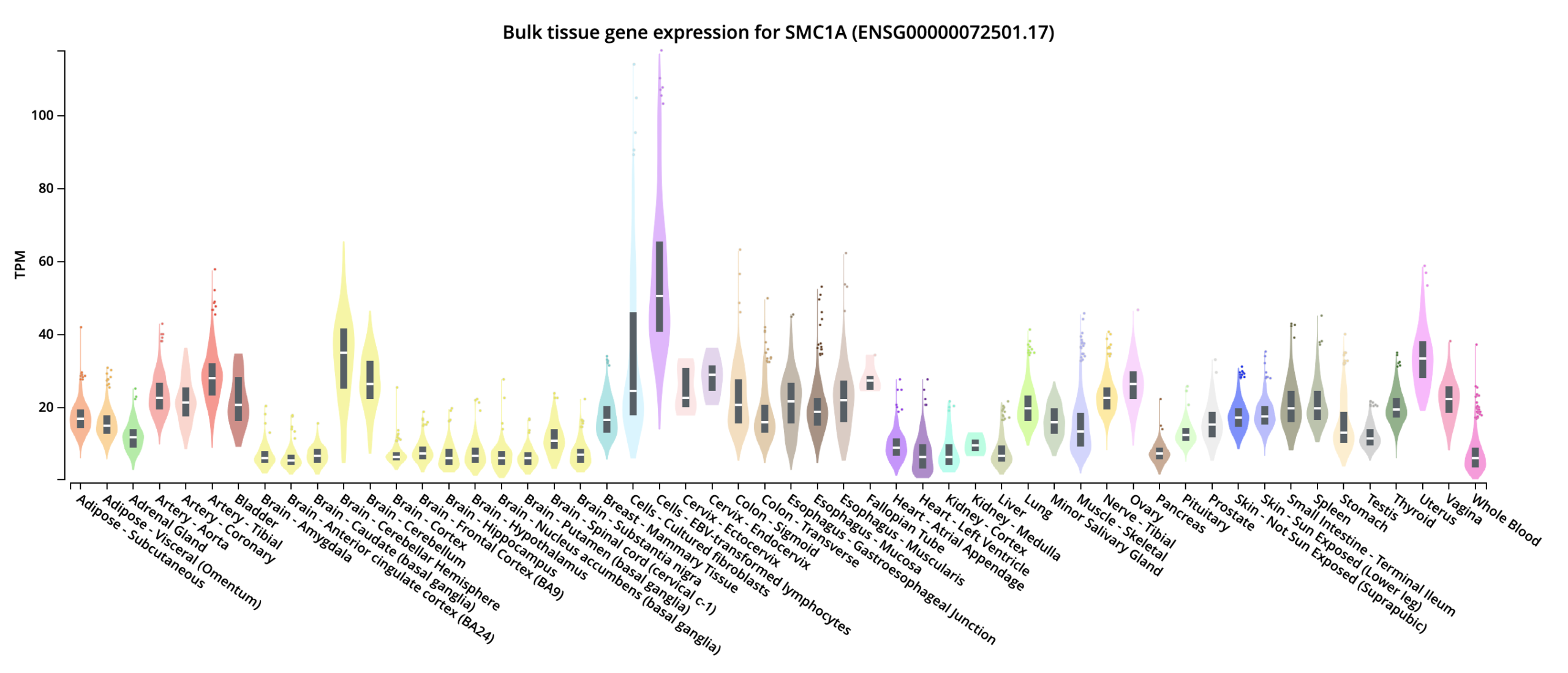
Every human has SMC1A gene in their body’s cells. This gene is responsible for producing SMC1A protein that’s critical for healthy and appropriate cell function.
The SMC1 protein is part of a larger protein group called the cohesin complex or cohesin ring.
If SMC1A gene works correctly, the cells perform appropriate function and body is healthy.
But people can have changes (variants/mutations) in SMC1A gene that lead to incorrect gene function and therefore, disease is caused.
Further, unlike males, Females have two X-chromosomes, two copies of the SMC1A gene in cells. One X-chromosome is silenced, other is active.
For affected individuals, the chromosome that’s silenced can have the healthy gene on it, and the chromosome that’s active, mutated gene. That’s why our disorder is called X-linked.
But the inactive x-chromosome can still releases some of the SMC1A protein in cells because SMC1A is reported to partially escape X inactivation (it is not classical escape) and for this unlike males, females tend to survive.
It is known that the amount of protein that’s released via inactive x-chromosome can vary from cell to cell.
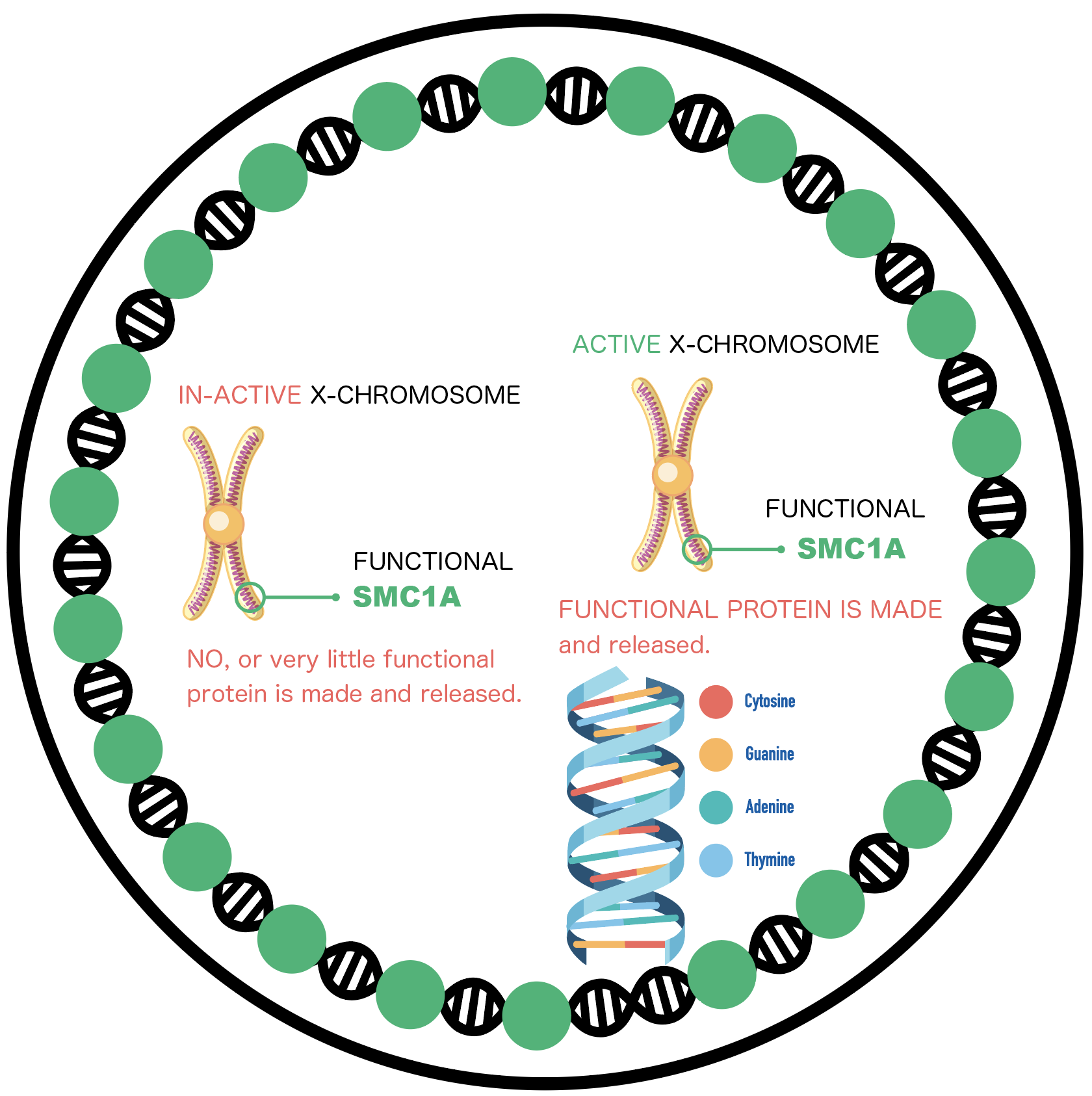
Functional HEALTHY CELL, with Functional SMC1A gene.

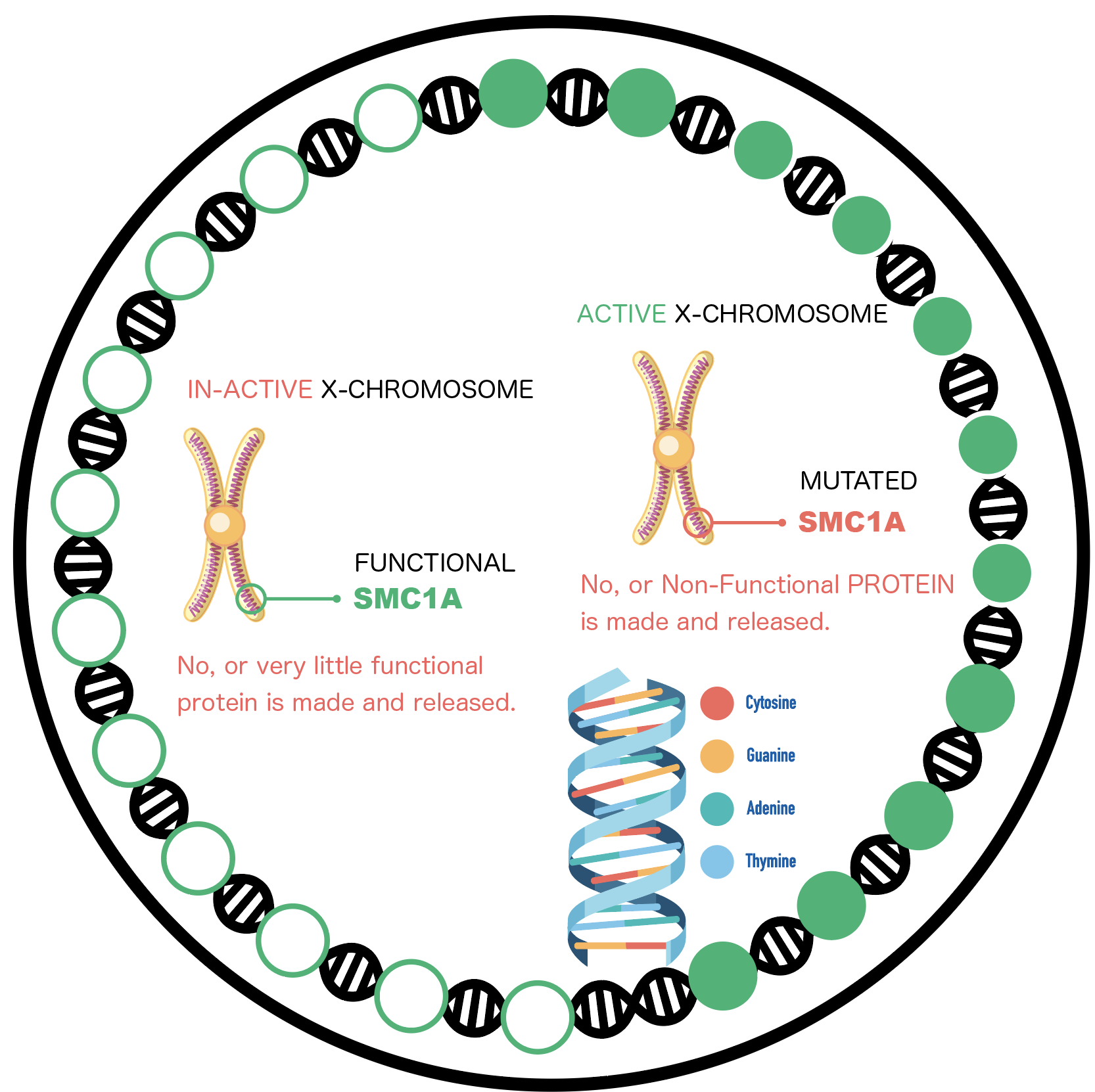
Non functional CELL, with Mutated SMC1A gene.
Lack of correct, functional protein in brain cells causes our disease – SMC1A DEE.
Not necessarily all cells in the Patient body have a non functional SMC1A.
Most SMC1A patients seem to have mosaicism. A person with mosaicism has a mixture of normal and mosaic DNA in the same type of cells, e.g. brain cells and throughout the body.
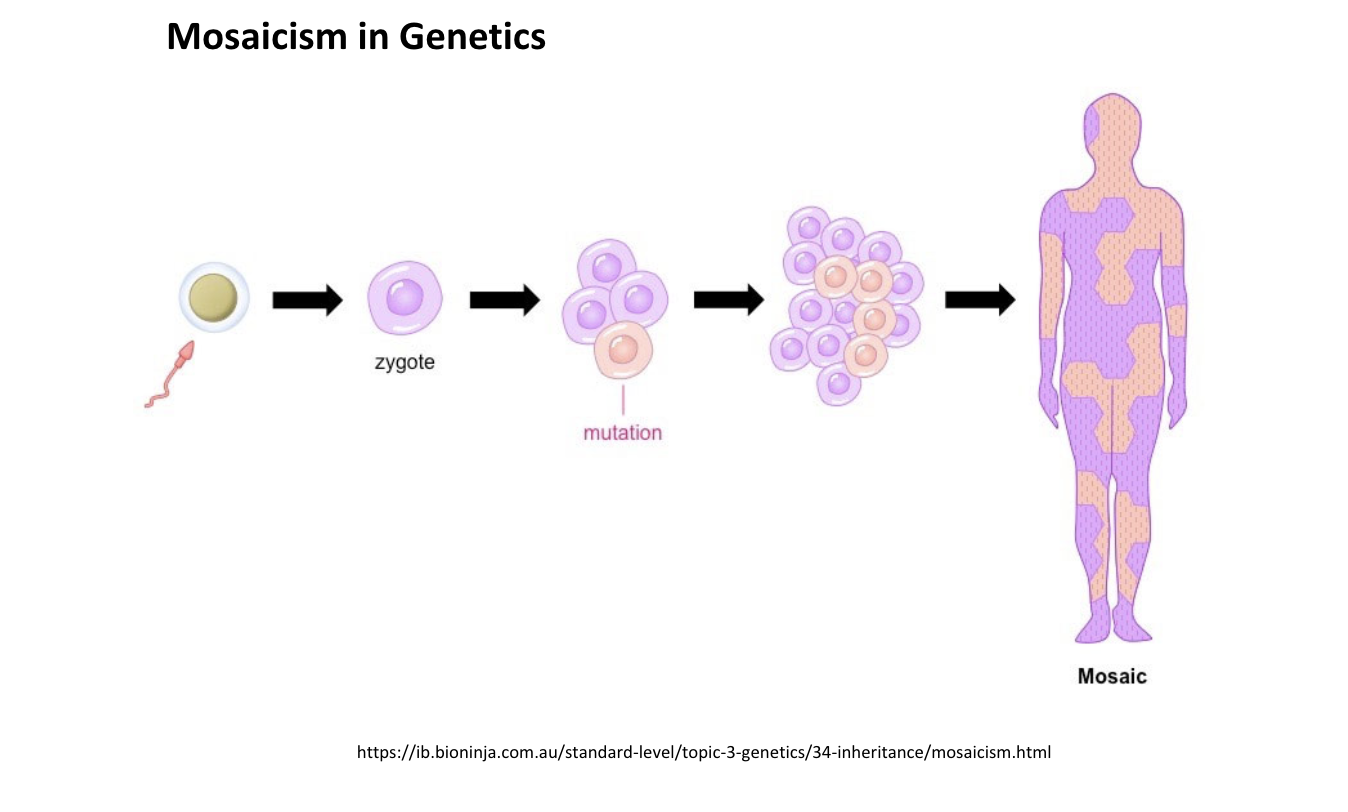
A zygote is a cell formed by a fertilization event.
Depending on the type of variants in the SMC1A, distinct disorders can result.
How is our group difference from CDLS?
Our group has type of mutations that cause lack of gene function, the gene does not make enough SMC1A protein and disrupts the cohesin ring. Either the ring is not formed or not enough protein is produced for it to be functional.
These mutations are called Loss of Function mutations and cause SMC1A related DEE that results in Intractable Seizures and Developmental Impairment.
In contrast, mutations that cause protein derangement or atypical arrangement in cells in cohesin ring, cause Cornelia de Lange Syndrome (CdLS), that has distinct clinical phenotype from our group.
The Significance of Our Girls
All the girls in this unique group have presumed loss of SMC1A function, caused by nonsense, frameshift or loss of function missense mutations, as well as a couple other mechanisms.
Neurodevelopmental Disorder caused by SMC1A Loss of Function, mostly characterized by intractable Epilepsy: Typical Phenotype
The majority of individuals with SMC1A Loss of Function have intractable epilepsy or hard to control seizures that present typically in clusters; all patients have developmental delays including disordered acquisition of cognitive and social competence, delays in reaching developmental milestones and general skills.
For now, Loss of Function variants in SMC1A appear to result from spontaneous (de novo) errors very early in embryonic development that occur for unknown reasons and are not inherited.
Every child is unique and the associated symptoms vary greatly in severity from case to case.
The typical phenotype can be characterized but is not limited by following symptoms.
- Global developmental delays and developmental impairment
- Intractable hard to control Seizures
- Autistic like features
- Balance and Coordination issues
- Sensory processing issues
- Motor planning difficulties
- Visual impairment or other vision related conditions
- Hearing impairment
- Growth deficiency
- Feeding and digestive challenges
- High (hypertonia) and low (hypotonia) muscle tones
- Musculoskeletal issues such as hyper mobility (lax joints)
- Sleep problems
- Reflux
- Behavioral Issues
- Anxiety
- Restricted, Repetitive Behaviors